Spiffin’ coronavirus vaccine
The purpose of a vaccine is effectively to train the immune system in recognising and combatting the virus quickly should there ever be a real infection. To do so, vaccines deliver virus components, which are harmless on their own, to the recipient’s immune system. These components are referred to as immunisation targets or immunogens. Once immune cells recognise and bind to these, an immune response follows.
There are a few different vaccine technology platforms in use or development. Here, I very briefly summarise the ones used for COVID-19 vaccines and then highlight one novel approach that has piqued my interest.
Vaccine development ideally targets highly conserved regions of a virus that are known to elicit an immune response. These are parts of the virus that it cannot afford to mutate too much because it risks losing its infectious power. For example, this could be a protein that enables the virus to attach to human cells to infect its new host (like the SARS-CoV-2 spike protein we keep hearing about – although this is known to mutate). Theoretically it is possible that there are transient virus versions that have significant mutations in such areas, but we might never know because those viruses have incapacitated themselves and, thus, never infect anyone or only few susceptible people.
Note that there is no intelligence behind these mutations. They simply happen and are either beneficial, detrimental or neutral for the virus. It does not decide to mutate.
COVID-19 vaccines
Currently, a few vaccines keep making the headlines, as they have made it onto the global market or are close. They fall into four technological categories. The vaccines from Pfizer-BioNTech and Moderna are mRNA-based. Oxford-AstraZeneca‘s, Johnson & Johnson/Janssen Pharmaceuticals‘, CanSino Biologics‘ and Russia’s Sputnik V use DNA vectors. All of these vaccines essentially deliver the genetic information necessary to instruct the recipient’s body to produce harmless virus components. The protein-based vaccines from GSK-Sanofi and Novavax aim to deliver ready-made virus components to the immune cells without the body having to build them first. The vaccines from Valneva, Sinopharm and Sinovac use inactivated coronavirus, which aims to provide the most native and complex presentation of virus material to the immune system. Presentation is key for a vaccine to be successful.
The spiffin’ vaccine
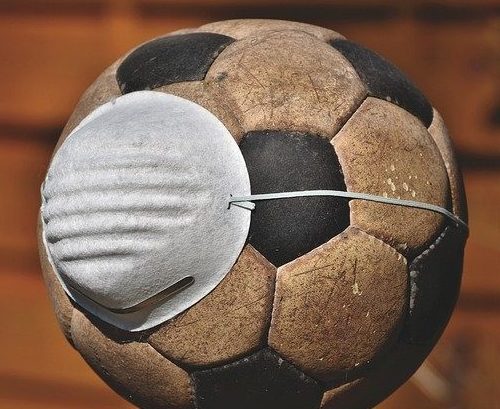
In amongst all the big news, I noticed an article about a protein-based COVID-19 vaccine candidate under development by the US Army. It is referred to as SpFN (spike ferritin nanoparticle). What piqued my interest was that the vaccine is multivalent, i.e. it can display multiple binding sites to immune cells on one vaccine molecule. Imagine a football where each hexagon and pentagon represents a binding site.
Why is this important?

The most effective protein-based vaccines so far have been those that mimic a virus structurally to some degree. This is possible through the use of technologies that facilitate the clustering of immunogens into small particles, i.e. nanoparticles. Immunogens are the parts of a virus that our immune cells need to detect to mount their defence. The superiority of nanoparticles over vaccines that use smaller molecules (soluble subunit vaccines) has been attributed to our immune system working best when it sees immunogens presented in a repetitive dense pattern just like on a real virus. Imagine looking at a 3D puzzle. You can maybe gauge what the final sculpture is supposed to be when the pieces are strewn across the floor, but once larger sections of the puzzle have been completed, you know much better what it’s meant to be. It is all about context, even for our immune cells.
A multivalent vaccine
SpFN employs ferritin as its key base component. This is a common protein in living organisms with 24 structural sites and is one of the better-researched platforms to create multivalent vaccines. It can be isolated from bacteria and engineered to suit in the lab. The idea of using ferritin as a vaccine particle base is not specific to COVID-19. It has also been researched for HIV-1 and influenza, for example.
Ferritin molecules can be fused to viral proteins. The resulting constructs self-assemble to form a virus-mimicking particle that displays viral proteins on its surface (think football). The result is a multivalent vaccine that offers a repetitive pattern of binding sites to stimulate immune cells. Research suggests that the use of more than one immunogen on the same ferritin construct may elicit cross-reactivity against related viruses, e.g. various coronaviruses.
It can be speculated that the use of more than one immunogen may also reduce the risk of vaccination failing due to virus mutations because one vaccine covers various viral targets. Thus, the chances are higher that the recipient mounts an immune response against several, if not all, of them. When the virus mutates one of those targets ‘in the wild’, the vaccinated human should still be able to defend themselves thanks to their immune system recognising other viral properties that have not mutated yet. This, in turn, would reduce the spread of new virus versions amongst the population and, ideally, mitigate further virus mutations. There will be limits of the number of viral proteins that can be used per ferritin construct, as the presentation density for each of them must be optimised to elicit a robust immune response.
In conclusion, vaccine nanoparticles offer a tool that enables us to present immunogens to immune cells in a 3D structure that mimics a real virus. If designed well, they elicit robust immune responses. One benefit is that there is no need for the use of inactivated viruses. Thus, this novel approach promises to be safer. Note that ferritin fusion is only one way of building vaccine nanoparticles. Novavax, for example, also employs nanoparticles in its COVID-19 vaccine but uses a different technology.
References
- HE, L., DE VAL, N., MORRIS, C.D., VORA, N., THINNES, T.C., KONG, L., AZADNIA, P., SOK, D., ZHOU, B., BURTON, D.R., WILSON, I.A., NEMAZEE, D., WARD, A.B. and ZHU, J., 2016. Presenting native-like trimeric HIV-1 antigens with self-assembling nanoparticles. Nature communications, 7, pp. 12041-12041.
- Khalili RA. 16/10/2020. MRDC. https://mrdc.amedd.army.mil/index.cfm/media/articles/2020/WRAIR_announces_COVID-19_vaccine_candidate
- MA, X., ZOU, F., YU, F., LI, R., YUAN, Y., ZHANG, Y., ZHANG, X., DENG, J., CHEN, T., SONG, Z., QIAO, Y., ZHAN, Y., LIU, J., ZHANG, J., ZHANG, X., PENG, Z., LI, Y., LIN, Y., LIANG, L., WANG, G., CHEN, Y., CHEN, Q., PAN, T., HE, X. and ZHANG, H., 2020. Nanoparticle Vaccines Based on the Receptor Binding Domain (RBD) and Heptad Repeat (HR) of SARS-CoV-2 Elicit Robust Protective Immune Responses. Immunity, 53(6), pp. 1315-1330.e9.
- POWELL, A.E., ZHANG, K., SANYAL, M., TANG, S., WEIDENBACHER, P.A., LI, S., PHAM, T.D., PAK, J.E., CHIU, W. and KIM, P.S., 2020. A single immunization with spike-functionalized ferritin vaccines elicits neutralizing antibody responses against SARS-CoV-2 in mice. bioRxiv, , pp. 2020.08.28.272518.
- ZHANG, B., CHAO, C.W., TSYBOVSKY, Y., ABIONA, O.M., HUTCHINSON, G.B., MOLIVA, J.I., OLIA, A.S., PEGU, A., PHUNG, E., STEWART-JONES, G., VERARDI, R., WANG, L., WANG, S., WERNER, A., YANG, E.S., YAP, C., ZHOU, T., MASCOLA, J.R., SULLIVAN, N.J., GRAHAM, B.S., CORBETT, K.S. and KWONG, P.D., 2020. A platform incorporating trimeric antigens into self-assembling nanoparticles reveals SARS-CoV-2-spike nanoparticles to elicit substantially higher neutralizing responses than spike alone. Scientific Reports, 10(1), pp. 18149.
1 thought on “Spiffin’ coronavirus vaccine”
Comments are closed.
[…] are a tool to assess how effective a vaccine is because a vaccine is supposed to stimulate an antibody-mediated immune […]